Can a mother with HIV breastfeed?
The Mother to Child Transmission of HIV
The transmission of HIV from the mother to the child can occur during pregnancy, childbirth and breastfeeding. The risk of transmission during pregnancy is about 7%. The risk during childbirth is up to 15%. And the risk during breastfeeding is also up to 15%.
WHO Recommendations
WHO has assisted each country to form guidelines to decide whether they will recommend breastfeeding while receiving appropriate medical interventions or they will avoid breastfeeding and recommend alternative feeding methods. Many developed countries recommend avoiding breastfeeding completely. India has adopted the policy for all mothers to breastfeed irrespective of their HIV status. Based on the new evidence, the WHO, for the first time, now recommends that HIV-positive mothers or their infants take antiretroviral drugs throughout the period of breastfeeding and until the infant is 12 months old. Recent studies have found that HIV transmission reduced to just 1.8% for infants given the antiretroviral drug nevirapine daily while breastfeeding for 6 months.
Revised WHO Recommendations on the use of antiretroviral drugs for treating pregnant women and preventing HIV infection in infants (2009)
The 2009 recommendations provide two alternative options for women who are not on
ART and breastfeed in resource-limited settings:
1) If a woman received AZT during pregnancy, daily nevirapine is recommended for her child from birth until the end of the breastfeeding period.
OR
2) If a woman received a three-drug regimen during pregnancy, a continued regimen of triple therapy is recommended through the end of the breastfeeding period.
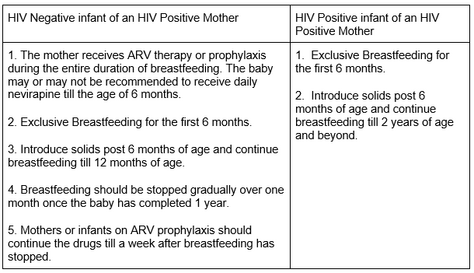
Some specific guidelines followed in India are given in the table below.
The Option of Alternative or Replacement Feeding
Many developed countries including the USA have adopted the policy to avoid breastfeeding completely when the mother is HIV positive. In these countries, the state supports infant feeding. There is access to alternatives and clean water etc. In India, if HIV positive Mothers from high income families choose not to breastfeed, replacement feeding can be advocated. This option is chosen on the following AFASS criteria.
A– Acceptable
F– Feasible
A – Affordable
S– Safe
S– Sustainable
When the mother chooses not to breastfeed, her options of alternative feedings are the following.
- Expressed heat-treated breastmilk (this is an option even when a breastfeeding HIV positive mother is facing temporary issues like mastitis, unavailability of ARV drugs etc)
- Breastfeeding by another HIV negative woman (wet nursing)
- Human breast milk from breast milk banks.
- Commercial Formula
- Animal milk (after the baby has completed 6 months)
What not to do?
- Do not do mixed feeding (breastfeeding + top milk). It increases the risk of HIV transmission 3 to 4 times. Therefore, the baby should be either exclusively breastfed or exclusively fed by alternative methods. Mixed feeding should be avoided under every circumstance.
- Do not let Nipple fissures, engorgement or mastitis develop. In order to do this, ensure lactation support right from the beginning.
- Do not let bacterial infections such as thrush develop in the baby or the mother. Hygiene practices should be followed very dedicatedly.
- Do not combi-feed during the temporary problems mentioned above. Use the option of expressed heat-treated breast milk.
References
IYCN Course, BPNI Maharashtra
https://www.who.int/elena/titles/hiv_infant_feeding/en/
https://www.who.int/bulletin/volumes/88/1/10-030110/en/
https://www.unicef.org/nutrition/files/Global_Breastfeeding_Collective_Advocacy_Brief_Breastfeeding_and_HIV.pdf
https://www.bpni.org/hiv/hiv_if_principles_recommendations_112009.pdf

Wish to speak with a member of our team who is a certified lactation professional and also an experienced breastfeeding mother, click on this link.
Medical Advice Disclaimer
THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Disclaimer
We understand and acknowledge that parents and babies can be of various genders on a spectrum of LGBTQI+. Families come in diverse flavours. However, in our articles, for the sake of simplicity and convenience, we will be referring to the breastfeeding parent as the mother and using the female pronouns- ‘she’ and ‘her’ for babies. Babies can be nourished and nurtured in different ways and while we have used the terms breastfeeding and nursing, we recognize that parents can opt to chest feed or finger feed.
We don’t have conflicts of interest and declare, and we are compliant with the WHO code of marketing of breastmilk substitutes and the IMS act.
In case you find any information on this website that needs to be updated, please write to us at info@bsim.org.in






