I feel depressed/sad/angry/put off by breastfeeding, what is happening?
Nursing aversion or Breastfeeding aversion and agitation is a phenomenon that some women experience in their breastfeeding journey. It is an experience marked with negative feelings and intrusive thoughts while the baby is latched on and is breastfeeding.
Signs:
Mothers who experience nursing aversion often report experiencing the following negative feelings and intrusive thoughts while breastfeeding.
- Irritability
- Agitation
- Anger
- Rage
- The sensation of skin itching and crawling
- An overwhelming urge to stop breastfeeding
- The feeling of being touched out
- The feeling of being trapped
- A wish to run away or escape to avoid breastfeeding
- An urge to unlatch, pinch or push the baby so she would stop breastfeeding
These feelings and thoughts occur only while breastfeeding and when the baby stops nursing, they go away. However, the intensity and duration vary from mother to mother. Most mothers experience feelings of guilt and shame afterward.
Causes:
There is no research done on the phenomenon of nursing aversions to determine its causes. And therefore, the data available is anecdotal and not based on research studies. Following are the probable causes for BAA.
1. Hormonal Reasons
a. Menstruation – A lot of women who experience aversion, experience it around their periods. Usually, from the onset of periods (a couple of days before it starts) continuing till the periods start or sometimes till a couple of days into the period.
b. Ovulation – Some women experience nursing aversion around the time they ovulate.
c. Pregnancy – The hormonal changes that pregnancy brings about potentially cause nursing aversion in a lot of women.
2. Lack of Self-care
a. Sleep Deprivation – All new mothers expect to get less sleep. But what is not discussed much is that for some mothers, the sleep deprivation goes on for years. It is not unreasonable to deduce that incessant sleep interruptions and deprivation could cause symptoms of BAA.
b. Lack of Nutrition and Poor Hydration – A lot of women have reported that when they took supplements for their deficiencies of magnesium, iron, vitamin A, B complex and D, it helped a lot in their BAA symptoms. It can be hypothesized that these deficiencies could be contributing to nursing aversion. Drinking more water too has been reported to bring a decrease in BAA symptoms making lack of hydration a plausible cause of aversion.
c. Exhaustion – The physical and mental exhaustion of being the primary caregiver can be immense. Not getting any me-time or a break from the constant chores and responsibilities can sometimes trigger BAA.
3. Mental Health
a. Postpartum Depression (PPD) – There seems to be a close relation between PPD and BAA. PPD can cause symptoms like anger/agitation, anxiety, irritability which in turn can trigger an aversion.
b.Stress – Maternal stress can be sensed by the baby and causes stress in the baby too. It is known that the stress hormone ‘cortisol’ can pass through breast milk. According to a theory, when a transfer of stress happens from the mother to the infant, it causes the baby to nurse more frequently and for longer duration, potentially causing more stress in the mother which again is passed to the baby. This cycle goes on and can trigger aversion.
4. Breastfeeding Factors
a. Pain – Persistent pain while breastfeeding (due to a poor latch or any other reason) can lead to BAA.
b. Tandem feeding Newborn and Older child – A newborn feeds like a newborn: very frequently, marked with long stretches of cluster feeding. It is exhausting in itself. When there is an additional demand from the older child as well, it can be very challenging. Some women have reported feeling averse to nursing due to the overwhelmingness of tandem feeding.
5. Previous History of Sexual Abuse
a. Childhood Sexual Abuse (CSA) – A history of childhood sexual abuse can affect a woman’s experience of breastfeeding. In some cases, it may promote healing; however, in some others, it could be emotionally very triggering. In such cases, the woman may develop BAA.
b. Sexual Abuse during adolescence and adulthood – Many women who were sexually abused during their teens, viewed their breasts as something that led to abuse. A positive body-image was a distant dream in the cases of such women. In their mind, their developing breasts were responsible for them being a victim of abuse. Such women were more likely to stop breastfeeding due to the emotional upheaval they felt while nursing. Many felt strongly averse to nursing.
Coping Strategies:
Nursing aversions are hard to ignore. At BSIM and in other breastfeeding communities, women have reported certain techniques that helped them. These techniques are best used for older babies (more than 1 year of age) who do not exclusively depend on breastfeeding.
Some coping strategies are listed below.
1. Distracting the baby –
Distracting the baby with a favorite toy or book or some other interesting activity when the mother is not up for breastfeeding or when she wants to end the session is a useful technique.
2. Distracting Self –
Many women have tried distracting themselves by reading a book or immersing themselves in the screen (TV/Phone) while nursing. It helps them get through the session.
3. Addressing the cause –
If a mother can find out the real cause of her aversion, she can work through it with the help of therapy (for reasons like sexual abuse) or medication (if need be, for reasons like PPD or other mood disorders).
4. Improving Diet and Taking Supplements for Deficiencies –
Having a balanced diet and taking supplements for deficiencies of magnesium, vitamins and iron can help.
5. Predicting and Anticipating –
Women who experience aversion at particular times like while ovulating and/or menstruation can predict their aversion and tackle it with their awareness of the fact that it will disappear.
6. Setting Boundaries –
Boundary-setting for skipping or shortening nursing sessions works well while a mother deals with her aversion. Some commonly used techniques are ending the nursing session at the end of counting 1 to 10, Not asking to nurse when the mother is sitting on a particular chair or sofa (the no-nursing zone) etc. More techniques that are used while weaning a baby can be adapted to the situation and used. For more ideas, click here.
7. Taking help from the non-breastfeeding parent and other family members/friends –
This is extremely crucial during bouts of intense aversion. The mother can ask her spouse/partner/family/friends to distract/engage the baby.
8. Partial Weaning –
Sometimes day or night weaning (whichever is more triggering) can help a great deal and the mother can continue nursing while addressing her aversion.,
9. Weaning –
In some cases, women have chosen to wean the baby to maintain their own sanity and calm. Breastfeeding is a relationship involving two parties and the mother’s needs are equally important. Also, if a breastfeeding relationship is potentially affecting an overall relationship between the mother and the baby adversely; it makes sense to end it. When used as a last resort, weaning is justified and should not bring shame or guilt to the mother.
10. Other Techniques –
Some women have found help from positive affirmations and by doing healthy and favorite activities (showering/writing etc) to keep oxytocin flowing in order to minimize their nursing aversion.
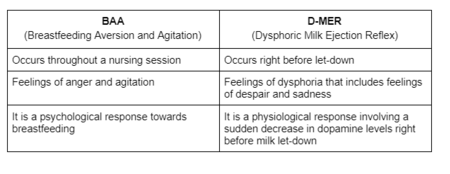
BAA vs D-MER:
BAA is often confused with D-MER. But it is important to note that these are two different phenomena. However, it is possible for a mother to experience both at the same time.
References:
https://kellymom.com/bf/concerns/mother/breastfeeding-nursing-aversion-agitation-baa/
https://www.laleche.org.uk/dont-enjoy-breastfeeding/
https://www.breastfeedingaversion.com/what-is-nursing-aversion
https://www.breastfeedingaversion.com/theories-of-causation1
https://lllusa.org/breastfeeding-aversion-what-helped-you/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2860840/
https://mamasmilknochaser.com/2018/10/04/breastfeeding-with-a-history-of-sexual-abuse-women-speak/
Wish to speak with a member of our team who is a certified lactation professional and also an experienced breastfeeding mother, click on this link.
Medical Advice Disclaimer
THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Disclaimer
We understand and acknowledge that parents and babies can be of various genders on a spectrum of LGBTQI+. Families come in diverse flavours. However, in our articles, for the sake of simplicity and convenience, we will be referring to the breastfeeding parent as the mother and using the female pronouns- ‘she’ and ‘her’ for babies. Babies can be nourished and nurtured in different ways and while we have used the terms breastfeeding and nursing, we recognize that parents can opt to chest feed or finger feed.
We don’t have conflicts of interest and declare, and we are compliant with the WHO code of marketing of breastmilk substitutes and the IMS act.
In case you find any information on this website that needs to be updated, please write to us at info@bsim.org.in






